Types of Arthritis Causing Ankle Pain
 There are many kinds of arthritis, and one of them could be a cause of your ankle pain. Osteoarthritis, the most common type, occurs when wear and tear on the cartilage that cushions the ends of the bones causes the bones to rub against each other. People with osteoarthritis in their ankle may experience painful joints between the shin and ankle. Rheumatoid arthritis, an autoimmune condition, often causes joint pain in both ankles. Gout is another type of arthritis that can cause ankle pain because of a buildup of uric acid in the body. Gout patients often feel pain in the big toe as one of their first symptoms. Sudden intense pain that lasts for several hours and affects any of the joints, including ankles, can indicate a gout attack. These are not the only forms of arthritis that can lead to ankle pain. Understanding the specific type of arthritis affecting the ankle is important for developing an effective treatment plan. If you are experiencing persistent ankle pain, it is suggested you consult a podiatrist who can help identify the underlying cause of your pain, diagnose types of arthritis, and explore appropriate treatment plans.
There are many kinds of arthritis, and one of them could be a cause of your ankle pain. Osteoarthritis, the most common type, occurs when wear and tear on the cartilage that cushions the ends of the bones causes the bones to rub against each other. People with osteoarthritis in their ankle may experience painful joints between the shin and ankle. Rheumatoid arthritis, an autoimmune condition, often causes joint pain in both ankles. Gout is another type of arthritis that can cause ankle pain because of a buildup of uric acid in the body. Gout patients often feel pain in the big toe as one of their first symptoms. Sudden intense pain that lasts for several hours and affects any of the joints, including ankles, can indicate a gout attack. These are not the only forms of arthritis that can lead to ankle pain. Understanding the specific type of arthritis affecting the ankle is important for developing an effective treatment plan. If you are experiencing persistent ankle pain, it is suggested you consult a podiatrist who can help identify the underlying cause of your pain, diagnose types of arthritis, and explore appropriate treatment plans.
Ankle pain can be caused by a number of problems and may be potentially serious. If you have ankle pain, consult with Dr. Barbara Davis from Gilbert Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Ankle pain is any condition that causes pain in the ankle. Due to the fact that the ankle consists of tendons, muscles, bones, and ligaments, ankle pain can come from a number of different conditions.
Causes
The most common causes of ankle pain include:
- Types of arthritis (rheumatoid, osteoarthritis, and gout)
- Ankle sprains
- Broken ankles
- Achilles tendinitis
- Achilles tendon rupture
- Stress fractures
- Bursitis
- Tarsal tunnel syndrome
- Plantar fasciitis
Symptoms
Symptoms of ankle injury vary based upon the condition. Pain may include general pain and discomfort, swelling, aching, redness, bruising, burning or stabbing sensations, and/or loss of sensation.
Diagnosis
Due to the wide variety of potential causes of ankle pain, podiatrists will utilize a number of different methods to properly diagnose ankle pain. This can include asking for personal and family medical histories and of any recent injuries. Further diagnosis may include sensation tests, a physical examination, and potentially x-rays or other imaging tests.
Treatment
Just as the range of causes varies widely, so do treatments. Some more common treatments are rest, ice packs, keeping pressure off the foot, orthotics and braces, medication for inflammation and pain, and surgery.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Definition and Symptoms of an Achilles Tendon Injury

The Achilles tendon, a strong band of tissue connecting the calf muscles to the heel bone, plays a pivotal role in facilitating movement. An Achilles tendon injury refers to the damage or inflammation that occurs in this critical structure, impacting the ability to walk, run, or perform various physical activities. Typically, injuries to the Achilles tendon manifest as pain, swelling, and stiffness, often concentrated near the back of the heel. Individuals may experience difficulty pointing their toes or pushing off the ground. The discomfort can range from mild to severe, and in some cases, a noticeable thickening of the tendon may be observed. Achilles tendon injuries are frequently associated with overuse, sudden increases in physical activity, or inadequate warm-up routines. If you have endured an Achilles tendon injury, it is suggested that you confer with a podiatrist who can guide you toward the correct treatment method.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact Dr. Barbara Davis of Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Podiatry and Rheumatoid Arthritis

Podiatry is a specialized medical field dedicated to evaluating, diagnosing, and addressing issues related to the feet and ankles. Practitioners who hold specialized or extended roles in podiatry are well-equipped to provide expert assessment, guidance, and treatment for individuals dealing with all types of foot and ankle problems, including rheumatoid arthritis, or RA. Among patients affected by RA, podiatric care is a highly sought-after service. Podiatrists possess the knowledge and skills required to understand the unique challenges posed by rheumatic diseases on the feet and ankles. These doctors play a critical role in managing the foot-related aspects of RA, offering patients comprehensive care to alleviate pain, improve mobility, and enhance their overall quality of life. If you suffer from rheumatoid arthritis that is impacting your feet and ankles, it is suggested that you schedule an appointment with a podiatrist for treatment.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Dr. Barbara Davis of Gilbert Podiatry. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes and Symptoms of Turf Toe

Turf toe is a common injury that often strikes athletes such as football players, dancers and gymnasts, with a sudden and traumatic onset. Most recall the precise moment it occurred. Turf toe results in pain around the ball of the foot, particularly on the bottom of the metatarsophalangeal, or MTP, joint, just below the big toe. Those experiencing turf toe may note pain with or without movement. It can be felt when the toe is flexed to the extreme or during the toe-off phase of walking. Swelling of the MTP joint may accompany the pain, along with a decrease in strength and range of motion. The affected joint also may become warm and tender to the touch. Turf toe can cause a noticeable lump or gap, and what is described as a crunchy feeling due to inflammation. Difficulty walking and maintaining balance can result from the pain and loss of function in the affected joints and surrounding tissues. If you suspect a turf toe injury, it is suggested that you schedule an appointment with a podiatrist for an exam and accurate diagnosis. A tailored treatment plan can help you get back in the game.
Toe pain can disrupt your daily activities. If you have any concerns, contact Dr. Barbara Davis of Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Causes Toe Pain?
Most severe toe pain is caused due to a sports injury, trauma from dropping something heavy on the toe, or bumping into something rigid. Other problems can develop over time for various reasons.
Toe pain can be caused by one or more ailments. The most common include:
- Trauma
- Sports injury
- Wearing shoes that are too tight
- Arthritis
- Gout
- Corns and calluses
- Hammertoe
- Bunions
- Blisters
- Ingrown toenails
- Sprains
- Fractures (broken bones)
- Dislocations
When to See a Podiatrist
- Severe pain
- Persistent pain that lasts more than a week
- Signs of infection
- Continued swelling
- Pain that prevents walking
Diagnosis
In many cases the cause of toe pain is obvious, but in others, a podiatrist may want to use more advanced methods to determine the problem. These can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatments for toe pain and injuries vary and may include shoe inserts, padding, taping, medicines, injections, and in some cases, surgery. If you believe that you have broken a toe, please see a podiatrist as soon as possible.
If you have any questions please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What Is a Diabetic Foot Ulcer?
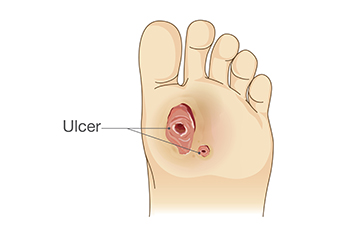
A diabetic foot ulcer, a grave complication for individuals with diabetes, is a chronic open sore that develops on the feet, typically on the bottom or sides. It arises from a combination of factors intricately linked to the effects of diabetes on the body. Diabetes can lead to neuropathy, causing reduced sensation in the feet and making it challenging to detect injuries or pressure points. Additionally, compromised blood circulation hampers the healing process, increasing the risk of infections and the formation of ulcers. Contributing further, the elevated blood sugar levels associated with diabetes impair the immune system, increasing the risk of infections. Foot ulcers, if left untreated, can escalate into serious complications and be quite painful. Recognizing the effects of diabetic foot ulcers underscores the importance of meticulous foot care in diabetes management. If you have diabetes and have developed a foot ulcer, it is suggested that you are under the care of a podiatrist who can effectively treat this type of wound, and help you to manage this condition.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Barbara Davis from Gilbert Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diabetic Foot Blisters

Diabetic foot blisters are a rare, but distinctive complication of diabetes. They typically manifest as painless blisters on the feet of people with diabetes, often without an obvious cause like injury or friction. These blisters can resemble burn blisters, presenting a risk for infection, especially given the compromised wound-healing abilities associated with diabetes. The skin of diabetic patients is vulnerable due to a combination of poor circulation, diabetic neuropathy, and other skin complications like dryness and poor healing. Management of diabetic foot blisters involves careful monitoring to prevent infection, control of blood sugar levels to aid in healing, and protection from further injury. In most cases, they may resolve on their own with good diabetes management and proper foot care, which includes wearing well-fitting shoes and avoiding walking barefoot. However, if you are diabetic and have any new or worsening foot issues, it is strongly suggested that you make an appointment with a podiatrist to ensure timely and appropriate treatment.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Barbara Davis of Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
A Comprehensive Overview of Heel Spurs

Heel spurs, a common foot condition, are bony outgrowths that form on the underside of the heel bone. They often develop in response to long-term strain on the foot's ligaments and muscles. While many individuals have heel spurs, not all experience pain. When pain does occur, it is generally due to the inflammation of the surrounding tissues, a condition known as plantar fasciitis. The symptoms of heel spurs can include sharp, stabbing pain in the heel, especially while walking or standing after periods of rest. The pain tends to improve as the foot warms up but may return after prolonged activity. Risk factors for heel spurs include obesity, wearing poor-fitting or worn-out shoes, and activities that place excessive strain on the feet, such as running and prolonged standing. Diagnosis and treatment may involve having X-rays taken to confirm the presence of a heel spur. Understanding heel spurs and their management options is vital for individuals seeking relief from this often painful condition. If you have developed a heel spur, it is suggested that you consult a podiatrist who can determine if it is mild or severe, and offer treatment options that are right for you.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Dr. Barbara Davis from Gilbert Podiatry. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Gilbert, PA . We offer the latest in diagnostic and treatment technology to meet your needs.
Children’s Foot and Ankle Injuries

Children often experience foot and ankle injuries due to sports, games, or falls. These injuries can range in severity, requiring different levels of medical attention. Ankle sprains happen when ligaments in the ankle stretch or tear due to rapid movements, often occurring during sports or high-energy activities. This can lead to swelling, pain, and bruising. Ankle strains involve muscle overstretching or tearing, which can be acute or chronic. Severe strains need immediate medical attention. Sever's disease causes heel pain in growing children, worsening with high-impact activities. It generally resolves over time. Ankle fractures are common in sports, and may involve any ankle bone. Complex fractures may necessitate surgery. Other injuries like puncture wounds, compartment syndrome, and ankle dislocations can occur and should be promptly treated by a podiatrist. If your child has a foot or ankle injury, it is suggested that you schedule an appointment with a podiatrist for a diagnosis and proper treatment.
The health of a child’s feet is vital to their overall well-being. If you have any questions regarding foot health, contact Dr. Barbara Davis of Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tips for Keeping Children's Feet Healthy
- Make sure their shoes fit properly
- Look for any signs of in-toeing or out-toeing
- Check to see if they have Clubfoot (condition that affects your child’s foot and ankle, twisting the heel and toes inward) which is one of the most common nonmajor birth defects.
- Lightly cover your baby’s feet (Tight covers may keep your baby from moving their feet freely, and could prevent normal development)
- Allow your toddler to go shoeless (Shoes can be restricting for a young child’s foot)
- Cut toenails straight across to avoid ingrown toenails
- Keep your child’s foot clean and dry
- Cover cuts and scrapes. Wash any scratches with soap and water and cover them with a bandage until they’ve healed.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Risk Factors for Peripheral Artery Disease

Peripheral arterial disease, or PAD, is a vascular condition characterized by narrowed arteries in the legs, limiting blood flow to the feet. Several risk factors contribute to the development and progression of PAD. Smoking is a primary risk factor, as it damages blood vessels and promotes plaque buildup. Diabetes is another significant factor, as high blood sugar levels can damage arteries. Hypertension, or high blood pressure, places constant stress on arteries and can lead to their narrowing over time. Age is also a non-modifiable risk factor, as PAD becomes more common with advancing age. Genetics can play a role, with a family history of vascular diseases increasing one's susceptibility. Obesity and a sedentary lifestyle contribute by promoting the accumulation of fatty deposits in arteries. Additionally, high cholesterol levels can lead to plaque formation in blood vessels. Lastly, individuals with a history of heart disease are at higher risk for PAD. If you have risk factors for PAD or suffer from its effects on your feet, it is suggested that you schedule an appointment with a podiatrist for an examination and necessary treatment.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Barbara Davis from Gilbert Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
More...
Can Overpronation Be Corrected?
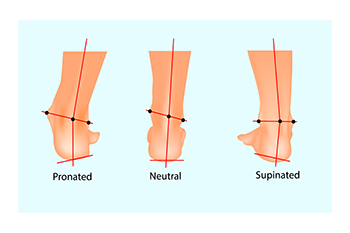
Overpronation, a common foot condition involving excessive inward rolling, requires careful attention to alleviate symptoms and prevent complications. The primary approach to overpronation involves adopting supportive footwear, which may include specialized shoes to minimize excessive movement and provide stability in the heel and midfoot. For those with moderate to severe overpronation, custom orthotics, tailored to the individual's foot shape, provide personalized assistance in reducing overpronation. Targeted exercises are believed to help in correcting overpronation. The short-foot exercise, involving lifting the arch of the foot off the ground, is particularly beneficial in addressing overpronation. In rare cases of severe overpronation, surgical intervention may be necessary. Reconstruction surgery aims to realign bones, providing better arch support, and may involve the use of stabilizing metal implants. If overpronation affects your well-being, it is suggested that you make an appointment with a podiatrist for a gait analysis, examination, and a treatment plan targeted to your particular condition.
If you have any concerns about your feet, contact Dr. Barbara Davis from Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Early Indicators of Foot Arthritis
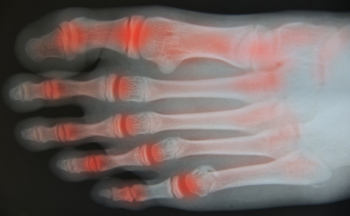
Foot arthritis, a condition affecting the joints in the feet, often begins its onset with inconspicuous signs that warrant attention. Persistent morning stiffness, particularly in the feet, can be an early red flag. Individuals may notice increased discomfort during weight-bearing activities or difficulty flexing and extending the foot joints. Swelling and warmth around the joints may accompany these symptoms, indicating inflammation. As arthritis progresses, subtle changes in foot structure or the development of bunions and hammertoes may become noticeable. Gradual limitations in range of motion may hinder daily activities. Persistent pain, even at rest, is another key signal that warrants investigation. Recognizing these initial whispers of foot arthritis allows for early intervention, potentially mitigating the impact on mobility and overall quality of life. If you have symptoms of foot arthritis, it is strongly suggested that you are under the care of a podiatrist who can effectively diagnose and offer treatment and relief options.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Barbara Davis from Gilbert Podiatry. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a joint disorder that involves the inflammation of different joints in your body, such as those in your feet. Arthritis is often caused by a degenerative joint disease and causes mild to severe pain in all affected areas. In addition to this, swelling and stiffness in the affected joints can also be a common symptom of arthritis.
In many cases, wearing ill-fitting shoes can worsen the effects and pain of arthritis. Wearing shoes that have a lower heel and extra room can help your feet feel more comfortable. In cases of rheumatoid arthritis, the arch in your foot may become problematic. Buying shoes with proper arch support that contour to your feet can help immensely.
Alleviating Arthritic Pain
- Exercises that stretch the foot can prevent further pain and injury and increase mobility
- Most of the pain can be alleviated with anti-inflammatory drugs, heat, and topical medications
- Massages can help temporarily alleviate pain.
It is best to see your doctor for the treatment that is right for your needs and symptoms. Conditions vary, and a podiatrist can help you determine the right method of care for your feet.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Effective Stretches for Improved Heel Stability

Heel stability is an important aspect of overall balance and comfort, and it is often overlooked until you experience pain or discomfort in that area. Fortunately, there are several stretches that can help enhance heel stability and promote overall foot health. One beneficial stretch is the calf stretch. This simple exercise involves extending one leg behind you and leaning forward with the other, feeling the stretch in your calf and Achilles tendon. By keeping these areas flexible, you reduce the strain on your heel. Another effective stretch is the plantar fascia stretch. To perform this, sit down and cross one ankle over the opposite knee. Gently pull your toes back toward your shin, feeling the stretch along the arch of your foot. This stretch helps to maintain the flexibility of the plantar fascia, thus reducing the risk of heel pain. The final stretch to consider is the toe stretch. This can be done by sitting or standing and extending your toes as far as possible, then curling them under. This exercise strengthens the muscles in your feet and enhances overall heel stability. If you would like additional information about effective heel stability stretches, it is suggested that you speak with a podiatrist who can provide you with the knowledge you are seeking.
Why Stretching Is Important for Your Feet
Stretching the feet is a great way to prevent injuries. If you have any concerns with your feet consult with Dr. Barbara Davis from Gilbert Podiatry. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Stretching the Feet
Stretching the muscles in the foot is an important part in any physical activity. Feet that are tight can lead to less flexibility and make you more prone to injury. One of the most common forms of foot pain, plantar fasciitis, can be stretched out to help ease the pain. Stretching can not only ease pain from plantar fasciitis but also prevent it as well. However, it is important to see a podiatrist first to determine if stretching is right for you. Podiatrists can also recommend other ways to stretch your feet. Once you know whether stretching is right for you, here are some excellent stretches you can do.
- Using a foam roller or any cylindrical object (a water bottle or soda can will do), roll the object under your foot back and forth. You should also exert pressure on the object. Be sure to do this to both feet for a minute. Do this exercise three times each.
- Similar to the previous exercise, take a ball, such as a tennis ball, and roll it under your foot while seated and exert pressure on it.
- Grab a resistance band or towel and take a seat. If you are using a towel, fold it length wise. Next put either one between the ball of your foot and heel and pull with both hands on each side towards you. Hold this for 15 seconds and then switch feet. Do this three times for each foot.
- Finally hold your big toe while crossing one leg over the other. Pull the toe towards you and hold for 15 seconds. Once again do this three times per foot.
It is best to go easy when first stretching your foot and work your way up. If your foot starts hurting, stop exercising to ice and rest the foot. It is advised that you then see a podiatrist for help.
If you have any questions, please feel free to contact our office located in Gilbert, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.